Ear Tube (Tympanostomy) Procedure
This surgery is done by an ear, nose, and throat (ENT) doctor or otolaryngologist. During surgery, the provider removes the fluid from your child’s middle ear and places a tiny tube in the eardrum. This tube creates a very small tunnel between the outer ear canal and the middle ear. This tunnel balances air pressure on both sides of the eardrum and prevents fluid buildup. In most cases, surgery can be done on both ears in less than 30 minutes. In some children, the adenoids are also taken out. The adenoids are small glands behind the nose and roof of the mouth. If adenoid problems are also being treated, surgery takes longer.
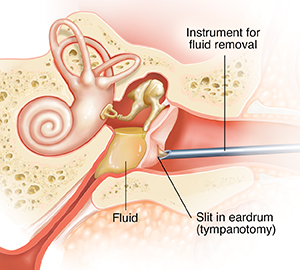
Making a slit
Most children are given general anesthesia so they will be asleep and comfortable during the procedure. Once your child is asleep, the ear canal is cleaned. Then the provider uses an operating microscope and special tools to make a small slit in the eardrum (tympanotomy).
Removing any fluid
A hollow tool is passed through the slit in the eardrum. Using gentle suction, the fluid is taken out through the tool. A fluid sample may be sent to a lab to figure out the cause of the fluid buildup, such as the type of bacteria that may be in the ear.
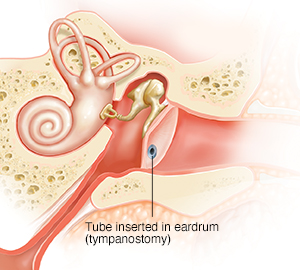
Putting in the tube
After the fluid is taken out, the healthcare provider puts a tiny tube into the same slit in the eardrum. The shape of the tube helps keep it in place.
The ENT specialist chooses the right tube for the best results. There are 2 types of ear tubes called short-term and long-term tubes. Most children have a short-term tube put in the eardrum. This type falls out on its own after several months. But it may last up to a year and a half. Long-term tubes often stay in place longer. A healthcare provider may need to take out a long-term tube.
Right after surgery
After surgery is done, your child will be taken to the postanesthesia care unit to be watched closely. Once fully awake and stable, your child should be able to go home. The tube may eventually fall out on its own over time. Follow up with your child's ENT healthcare provider as advised.
When to get medical care
Call your child's healthcare provider if any of the following occur:
-
Your child has ear pain, hearing loss, or problems with balancing or walking
-
Your child has bleeding from the ears
-
There is drainage from the ears after the first few days or increased drainage
-
Sticky or discolored fluid drains out of the ear after the first 48 hours
-
Your otherwise healthy child has a fever (see Fever and children, below)
-
Your child has had a seizure caused by the fever
-
You child is dizzy, confused, extremely drowsy, or has a change in mental state
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below is when to call the healthcare provider if your child has a fever. Your child’s healthcare provider may give you different numbers. Follow their instructions.
When to call a healthcare provider about your child’s fever
For a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
-
A fever of ___________as advised by the provider
For a child age 3 months to 36 months (3 years):
-
Rectal or forehead: 102°F (38.9°C) or higher
-
Ear (only for use over age 6 months): 102°F (38.9°C) or higher
-
A fever of ___________ as advised by the provider
In these cases:
-
Armpit temperature of 103°F (39.4°C) or higher in a child of any age
-
Temperature of 104°F (40°C) or higher in a child of any age
-
A fever of ___________ as advised by the provider